1. Introduction to Angina Pectoris and Myocardial Infarction
2. Understanding Angina Pectoris
Angina pectoris is a symptom of coronary artery disease characterized by chest pain or discomfort due to reduced blood flow to the heart muscle.
3. Characteristics of Angina Pectoris
Angina pectoris typically presents as pressure, squeezing, or tightness in the chest, although symptoms can vary in intensity and duration.
4. Types of Angina Pectoris
Angina pectoris can be classified into stable angina (predictable chest pain with exertion) and unstable angina (unpredictable chest pain at rest).
5. Causes of Angina Pectoris
Angina pectoris is caused by reduced blood flow to the heart muscle, usually due to narrowed or blocked coronary arteries.
6. Triggers of Angina Pectoris
Physical exertion, emotional stress, extreme temperatures, or heavy meals can trigger angina pectoris in susceptible individuals.
7. Diagnosis of Angina Pectoris
Diagnosis of angina pectoris involves a thorough medical history, physical examination, and diagnostic tests such as electrocardiogram (ECG), stress test, or coronary angiography.
8. Treatment of Angina Pectoris
Treatment for angina pectoris aims to relieve symptoms, prevent complications, and improve quality of life through medications, lifestyle modifications, and, in some cases, invasive procedures.
9. Understanding Myocardial Infarction (Heart Attack)
Myocardial infarction (MI) occurs when blood flow to a part of the heart muscle is blocked for an extended period, leading to tissue damage or death.
10. Characteristics of Myocardial Infarction
Myocardial infarction presents with severe and prolonged chest pain, often described as crushing or pressure-like, along with other symptoms such as shortness of breath, nausea, or sweating.
11. Types of Myocardial Infarction
Myocardial infarction can be classified into ST-segment elevation myocardial infarction (STEMI) and non-ST-segment elevation myocardial infarction (NSTEMI) based on electrocardiographic changes.
12. Causes of Myocardial Infarction
Myocardial infarction is usually caused by the rupture of a plaque in a coronary artery, leading to the formation of a blood clot that blocks blood flow to the heart muscle.
13. Risk Factors for Myocardial Infarction
Risk factors for myocardial infarction include hypertension, hyperlipidemia, diabetes, smoking, obesity, sedentary lifestyle, and family history of heart disease.
14. Diagnosis of Myocardial Infarction
Diagnosis of myocardial infarction involves a combination of clinical evaluation, electrocardiography (ECG), cardiac biomarkers (troponin), and imaging tests such as echocardiography or coronary angiography.
15. Treatment of Myocardial Infarction
Treatment for myocardial infarction aims to restore blood flow to the blocked artery as quickly as possible, typically through medications, percutaneous coronary intervention (PCI), or coronary artery bypass grafting (CABG).
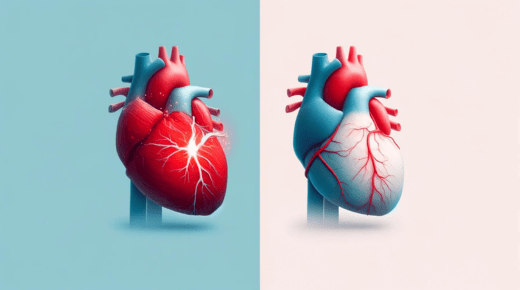
16. Key Differences Between Angina Pectoris and Myocardial Infarction
Angina pectoris is a symptom of reduced blood flow to the heart muscle, while myocardial infarction is a serious condition resulting from prolonged blockage of blood flow to a part of the heart.
Angina pectoris is usually relieved with rest or nitroglycerin, while myocardial infarction requires immediate medical intervention to prevent irreversible damage to the heart muscle.
17. Visual Representation of Angina Pectoris
Include diagrams or illustrations depicting the pathophysiology, symptoms, triggers, and treatment of angina pectoris.
18. Visual Representation of Myocardial Infarction
Include diagrams or illustrations illustrating the pathophysiology, symptoms, types, diagnosis, and treatment of myocardial infarction.
19. Risk Factors Comparison
Compare and contrast the risk factors associated with angina pectoris and myocardial infarction, highlighting common and unique risk factors for each condition.
20. Diagnostic Approach Comparison
Compare the diagnostic approach for angina pectoris and myocardial infarction, discussing the role of clinical evaluation, electrocardiography, cardiac biomarkers, and imaging tests in each condition.
21. Treatment Strategies Comparison
Compare and contrast the treatment strategies for angina pectoris and myocardial infarction, emphasizing the importance of timely intervention and individualized care.
22. Patient Education
Provide tips for patient education on recognizing the symptoms of angina pectoris and myocardial infarction, seeking prompt medical attention, and adopting heart-healthy lifestyle habits.
23. Healthcare Provider Guidance
Offer guidance for healthcare providers on distinguishing between angina pectoris and myocardial infarction, conducting appropriate diagnostic tests, and implementing evidence-based treatment strategies.
24. Conclusion
Summarize the key points discussed in the article and emphasize the importance of early recognition, accurate diagnosis, and prompt treatment of angina pectoris and myocardial infarction for optimal patient outcomes.
25. References
Provide a list of references for further reading, including textbooks, journal articles, and reputable online resources on angina pectoris, myocardial infarction, and cardiovascular health.